What is a Diabetic Retinopathy?
The effects of diabetes can have an impact on the eyes, just as in the body. In diabetic retinopathy, high blood sugar levels cause damage to the small blood vessels in the retina. Over time, these damaged vessels may leak fluid or blood, leading to swelling and vision problems. There are two main types of diabetic retinopathy: non-proliferative and proliferative.
-
- Non-proliferative Diabetic Retinopathy (NPDR): This is an earlier stage of the disease, where blood vessels in the retina have weakened and begin to leak, eventually leading to retinal swelling (edema). Symptoms of retinal edema include wavy or blurred vision, or new floaters.
- Proliferative Diabetic Retinopathy (PDR): Overtime, the progression of diabetic retinopathy can lead to “ischemic,” or unhealthy areas of retina that do not get enough blood supply. This is a more advanced stage where the body grows new, abnormal blood vessels in the retina’s surface, as a response to the growing ischemic regions. These new vessels are fragile and can bleed into the vitreous (back portion of the eye), causing large floaters or even significant vision loss.
How is a Diabetic Retinopathy Detected?
Diabetic retinopathy can progress without noticeable symptoms, therefore regular eye exams are essential for early detection. An ophthalmologist can detect diabetic retinopathy using various diagnostic testing, which may include:
-
- Dilated Retinal Examination: Drops are used to widen the pupils, allowing the doctor to view the retina more clearly.
- Fundus Photography: Special photographs of the retina can help document and monitor changes over time.
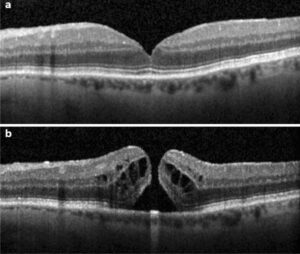
- Optical Coherence Tomography (OCT): This imaging test provides detailed cross-sections of the retina, helping to detect fluid accumulation and retinal damage.
- Fluorescein Angiography: A dye is injected into a vein in the arm, and photographs of the retina are taken as the dye travels through the blood vessels, highlighting any leakage or abnormal blood vessel growth.
 |
How is Diabetic Retinopathy Treated?
Treatment for diabetic retinopathy depends on the stage and severity of the disease:
-
- Early Treatment: In the non-proliferative stage, controlling blood sugar levels, blood pressure, and cholesterol can help prevent progression. Regular eye exams are crucial to monitor any changes.
- Laser Therapy: Laser treatment can help shrink abnormal blood vessels and reduce the risk of vision loss.
- Intravitreal Injections: Medications injected into the vitreous can help reduce retinal swelling and stop abnormal blood vessel growth. These medications include anti-VEGF (vascular endothelial growth factor) drugs and corticosteroids.
- Vitrectomy: In cases where bleeding into the vitreous has occurred, a surgical procedure called vitrectomy may be performed to remove the blood and scar tissue, helping to restore vision.
Managing Diabetic Retinopathy
Diabetic retinopathy requires ongoing management to prevent progression and preserve vision. Key steps include:
- Blood Sugar Control: Keeping blood glucose levels within the target range can significantly reduce the risk of developing diabetic retinopathy or slowing its progression.
- Regular Eye Exams: Routine eye exams are essential to catch any changes early and adjust treatment as needed.
- Lifestyle Changes: Maintaining a healthy diet, regular exercise, and controlling other health conditions like hypertension can improve overall outcomes.
If you have diabetes, it’s important to discuss any vision changes with your healthcare provider and schedule regular eye exams.
Do you have questions regarding Diabetic Retinopathy? Call us today! (561) 499-8830
Learn more about Diabetic Retinopathy:
National Eye Institute, NIH. Diabetic Retinopathy.
American Academy of Ophthalmology. Diabetic Retinopathy: Causes, Symptoms, Treatment.